Fourteen-year-old Nandini Chaturvedi from Madhya Pradesh’s Singrauli district is enjoying her favourite food, gets chatty and perky and flashes a warm smile when we meet her. She misses school though. That’s where she would meet her friends and romp around the playground. But it has been more than a year since she hasn’t met them. Over the past year she has been battling terminal cancer and extreme pain that had bound her to bed. But now, with palliative care at the cancer centre, AIIMS, Delhi, she is happy she can talk to them, engage in banter with her family at home and feel more whole than broken in the time she has left.
“Palliative care is medical caregiving aimed at optimising quality and dignity of life, mitigating pain and helping patients and family deal with a seemingly intractable situation with positivity. One of the challenges with terminal diseases is managing the expectations of the families and making the patients as comfortable as possible. Doctors are trained to treat patients, but they are not taught how to accept that someone is likely to die and ensure they die with dignity,” says Dr Sushma Bhatnagar, who heads the cancer centre at AIIMS and has been working to promote palliative care in the hospital. More than the pain-relieving medication, she and her team work on building trust with the family, reconcile with a possible outcome and build awareness on maximising the shared time they all have with terminal patients. Now Nandini’s family’s goals have changed. Initially, they wanted her to get better, walk and go back to school. They wanted her hair to grow so she could go back to tying ponies or plaits that she loved. Now, they want her to remain free of pain so that she can savour the food she eats, have a good night’s sleep and keep smiling for as long as she can. AIIMS is training doctors in 100 districts in North India so that sick patients do not have to travel far to access palliative services. Even Nandini, who has been receiving chemotherapy every 21 days since her treatment started in January, has to travel from Singrauli.

HOW NANDINI BECAME PAIN-FREE
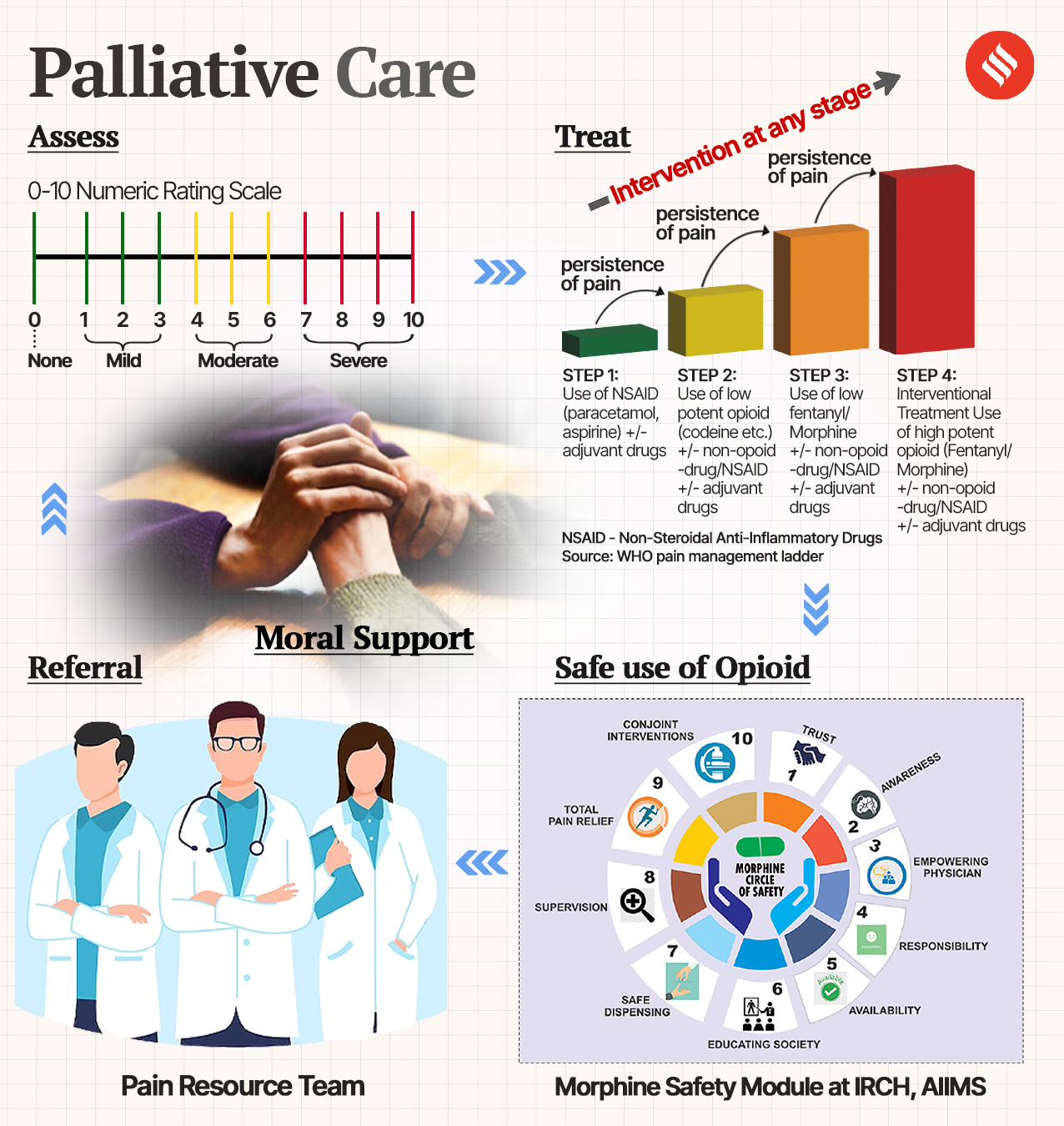
Last August, Nandini reported sharp pain in her left leg, which progressively worsened and crippled her. It was at AIIMS that she was detected with cancer in the left thigh bone. Her doctors knew that her prognosis was not very good. While the treatment continued, the palliative care team at the hospital stepped in to address her pain and to counsel the family on the possibility of her death. When none of the oral morphine pills worked, they gave her a strong, intravenous pain medication. “We broke the cycle of her pain. While she was not disease-free, she was pain-free. And that is very important for the patients as well as their family members. The AIIMS palliative care team uses a scale to quantify the pain of their patients – 0 being pain-free, 4 to 6 being moderate and 7 to 10 severe. At any stage of pain treatment, the first step is to prescribe the most common painkillers available. If the pain persists, a not-so-strong opioid is added to it. The third step on persistence of pain is to add a high potency pain killer. Then we prescribe an intravenous painkiller. Nandini’s pain was at level 10,” says Dr Bhatnagar. There are alternate pain therapies, too, like transcutaneous electrical nerve stimulation (TENS) or massage for lesser thresholds.
CONVINCING THE FAMILY: PRACTICAL DISEASE MANAGEMENT AND DIGNITY OF LIFE
The most important part about palliative care is to communicate with families about the possibility of death, accepting it and then planning to make the most of the time they have with their patient. “Any false hope leads to unnecessary therapies and health expenditure. We need the doctors to give a realistic picture to the patients and their family members and have conversations about how to make the patients as comfortable as possible. It is a group decision and determination to stay together without the isolating and cold confines of a hospital. If you see the ICUs in the cancer department, we do not see a single death there except for the unexpected ones. We counsel our patients to go home and spend their remaining time with family members instead of being restricted to the ICU where family members are not allowed most of the time,” says Dr Bhatnagar.
After staying at AIIMS for a couple of days to help doctors adjust her pain medication, Nandini’s parents take her home. They stay in touch with AIIMS doctors on the phone and bring her when the pain becomes unmanageable again. “It is a day care procedure, and we usually return the next day. This time, however, the pain that had subsided since her treatment at AIIMS, came back. She was back in her bed. She could not eat or speak. Now she is fine again,” says her mother Uma Chaturvedi.
HOW CAN THE AIIMS OUTREACH PROGRAMME HELP?
Most Read 1Chandrayaan-3 mission: Dawn breaks on Moon, all eyes on lander, rover to wake up 2As Indo-Canadian relations sour, anxiety grips Indian students, residents who wish to settle in Canada 3Karan Johar says Sanjay Leela Bhansali did not call him after Rocky Aur Rani: ‘He’s never called me but…’ 4Gadar 2 box office collection day 40: Hit by Shah Rukh Khan’s Jawan onslaught, Sunny Deol movie ends BO run with Rs 45 lakh earning 5Shubh’s tour in India cancelled: Why is the Canada-based singer facing the music?
AIIMS is now extending palliative care training to doctors, nurses and staff at healthcare facilities across 100 north Indian districts as part of the Government’s district-level palliative care programme. The shift will be from just disease management to post-disease rehabilitation and extension of quality of life. “First, we will be generating awareness of what it is, then we will be preparing the staff and teach them how to help families and patients come to terms with the most important component of palliative care, which is acceptance,” says Dr Bhatnagar, who is part of the training project in collaboration with the Indian Council of Medical Research (ICMR).
 (Source: IE Graphics)
(Source: IE Graphics)
The focus will be on communication. “We will train them how to talk to patients and families, explain the prognosis, counsel and prepare them. Then they will get to the physical part of the pain management module. They will be taught to grade pain and to resolve it by incrementally switching to more potent pain killers. The healthcare workers will be taught about educating the people on the use of morphine that also has high chances of addiction. I have had family members of patients who die bringing back leftover morphine. That’s because from the beginning itself we tell patients and their families about the dangers of the drug. They are taught not to share the prescription,” says Dr Bhatnagar. If district hospitals are empowered to manage pain on their own, then patients and families can resolve so much of their emotional, physical and financial stress.
Also ReadWeight loss is not just about cardio: Why you need strength training and …Why having leafy vegetables at the beginning of a meal can control your b…Is your bad cholesterol or LDL level not going down despite diet and exer…WHO hypertension report reveals 4.6 million lives in India can be saved b…
While palliative care is mostly associated with cancer and death, Dr Bhatnagar says that it doesn’t always entail end-of-life care. “Sometimes you need pain management for chronic conditions such as heart, kidney, or lung diseases,” she says, adding that she is working on promoting palliative care for other ailments as well.